Treatment Chart QA with MU/Gy plausibility checks
Quality Assurance of patient treatment parameters has to make sure that all patient related parameters in the treatment chart are as planned until the last treatment fraction is delivered. Even in an integrated system, human errors can occur, and also system related malfunctions cannot be excluded. Therefore, several checks are performed before the first treatment and during the course of the treatment:
Before the first treatment
When a 3D-treatment plan is approved ("plan approval"), it is printed and signed by a chief oncologist.
The plan is then checked by the medical physicist, who makes an independent monitor unit calculation and also signs the plan. Now the plan is ready for Simulation.
After the plan is simulated, all parameters are rechecked for consistency, correctness and completeness both by the physicist and by the oncologist. One of them approves the plan for treatment. Now all changes to relevant data are locked in the system. The patient chart and plan printout (which always is the "master" in case of inconsistencies) is transferred to the treatment machine.
At the linac, before the 1st treatment, the technologists again check that the database (RT-Chart) and the plan printout hold the same data.
During the first-day treatment, onclologist and physicist are present in the treatment room, again comparing the plan printout and the actual field setup parameters.
After the first treatment - chart checks
First of all, the oncologists review all port images taken for their patients. This can mean a lot of work: there are days where up to 200 images are acquired on our two machines. This image reviewing process is not discussed here. Instead, I want to focus on the plausibility checks, because I think this could (and should) be integrated into the system itself:
We have integrated the feature in a home-made report which is generated every morning by the physicists and which retrieves the patients who received a first-day treatment on the previous day. These patients are then opened in RT-Chart and checked immediately (in addition to the once-a-week check of all patients currently receiving treatments). For this first-day check, special attention is paid to the treatment history. The report contains a plausibility check for monitor units. If e.g. a certain treatment field with a field dose of 1Gy would contain 180MU, the report would highlight the MU-value. How does it work?
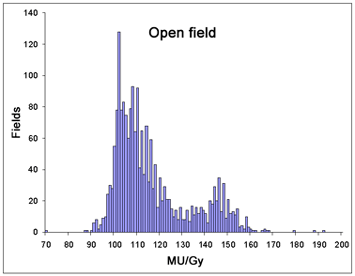
For non-IMRT treatments, 98% of our photon fields without beam modifiers (hard wedges, dynamic wedges) have MU-per-Gy values between 90 and 155 (with a peak at 102MU/Gy - the most probable value for supraclavicular fields, which are set up with SSD100). Therefore, actual MU/Gy values outside this range are highly suspicious. This does not mean automatically that an error has occurred: the placement of primary reference points sometimes gives reason for false alarm. But when the value is highlighted, the case will be investigated.
 |
Fig.1: Daily report, highlighting a suspicious MU value: The MU/Gy coefficient is not in the norm range specified in Tab.1. Click on image to enlarge.
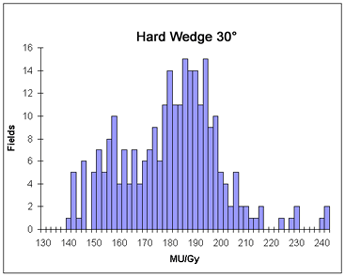
Evaluation of long-term MU/Gy statistics for all beam modifiers has resulted in norm ranges for all hard and dynamic wedges as well. But since the dynamic wedges have very similar "output factors", the plausibility check works better for the hard wedges.
| Beam modifier * | Norm range [MU/Gy] | Percentage of fields within norm range |
|---|---|---|
| None (open field) | 90 - 155 | 98% |
| Hard Wedge 15° | 120 - 170 | 95% |
| Hard Wedge 30° | 140 - 210 | 96% |
| Hard Wedge 45° | 185 - 285 | 95% |
| Hard Wedge 60° | 225 - 285 | 100%** |
| Enhanced Dynamic Wedge 10° | 120 - 150 | 95% |
| Enhanced Dynamic Wedge 15° | 120 - 150 | 94% |
| Enhanced Dynamic Wedge 20° | 125 - 155 | 96% |
| Enhanced Dynamic Wedge 25° | 125 - 155 | 95% |
| Enhanced Dynamic Wedge 30° | 120 - 160 | 98% |
Tab.1: Norm ranges for various beam modifiers, based on treatment statistics between 1.1.2004 and 1.2.2005.
Remarks:
*EDW angles 45° and 60° are not included here, because there are only single cases. Therefore statistics is poor.
**The Hard Wedge 60° also has poor statistics (only 10 fields).
Currently, the norm ranges include both photon energies (6MV, 15MV). The check could be refined (narrowing the norm ranges) by distinguishing between HiX and LoX. Further refinement could be done by dintinguishing between pelvic cases (having a rather high MU/Gy value for the lateral fields) and head&neck cases, where the isocenter depth is much less. Both information could easily be retrieved from the patient ID, which has a three character ending like HNO, PRO, ZNS, URO, ... which specifies the treatment region in most cases.
We think that this is a useful check which could always run in the background, and which should be integrated into a future version of RT-Chart, after the rules have been refined ("expert system").
 |
Fig.4: This is how a warning triggered by the expert system could look like.